EHRs are everywhere you see
… supporting clinical workflows in hospitals
… coordinating care across multiple clinics
… powering telehealth in digital health apps
And the list goes on…
AI-driven digital transformation has created opportunities for both providers and patients. In fact, the global Electronic Health Records market size is expected to reach $39.6bn with a 5.4% CAGR.
It doesn’t matter if it’s your first implementation or your tenth. In 2026, EHR systems are going to get a complete makeover.
The burning question right now is: Is your EHR system keeping up with the constant evolution of healthcare operations and patient care?
But before you answer that, you must know:
- Latest EHR trends shaping hospitals, clinics, and healthcare apps
- Healthtech dev practices to future-proof your custom EHR software
- Developer tips for secure, interoperable, and AI-enabled EHR systems
Don’t know these yet? This blog is worth a read!
What Is EHR?
EHRs, or electronic health records, are digital versions of a patient’s medical history. They include everything from diagnoses and lab results to medications and immunizations.
It’s not so surprising that they’re preferred nowadays. They provide a centralized, real-time view that makes care more coordinated, accurate, and efficient.
Table of Contents
And that’s not the only patient record management system out there. Understanding the difference between EHRs, EMRs, and PHRs helps you choose the right system for your healthcare needs.
Now that we know what EHRs are, let’s explore the latest trends that address the needs of the modern healthcare system.
What Are The Top EHR Trends To Look For In 2026?
The entire healthcare industry is changing with the introduction of novel technologies such as Agentic AI, AI-assisted robotics, and Generative AI. EHR is no different. Hospitals, clinics, and healthtech enterprises are already integrating these technologies.
Keeping an eye on the latest trends is crucial. And you don’t need to skim through the internet, as we’ve compiled the top five EHR trends for you. Here’s what’s on the horizon in 2026 and beyond.
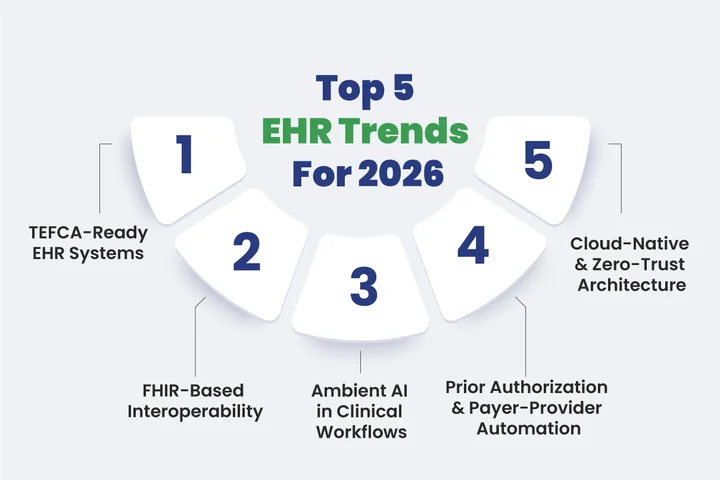
Trend #1: TEFCA-Ready EHR Systems
TEFCA (Trusted Exchange Framework & Common Agreement) is a set of standards designed to ensure the security, reliability, and consistency of electronic health record development and data exchange across healthcare organizations.
It lays the foundation for consistent EHR interoperability between hospitals, clinics, and digital health apps while protecting patient data and maintaining trust.
What happens when patient data doesn’t flow correctly between systems?
TEFCA solves this challenge by providing:
- Clear rules for secure, standardized data sharing
- Consistent protocols for consent and access management
- A framework that simplifies EHR development and integration
TEFCA-compliant EHRs use modern standards such as FHIR, which we’ll discuss next.
Trend #2: FHIR-Based Interoperability
FHIR implements TEFCA’s rules, enabling secure, real-time, and meaningful data exchange across healthcare systems. FHIR (pronounced ‘fire’) is an international standard for Fast Healthcare Interoperability Resources.
As per IBM’s Cost of a Data Breach Report 2025, the average healthcare breach costs around $9.77 million, making it the most expensive breach among all industries. That’s why exchanging data alone isn’t enough. You need FHIR-based interoperability.
Why use FHIR-native interoperability?
- It’s developer-friendly
- It’s built on modern web technologies like RESTful APIs, JSON, and XML
- It allows secure and coherent data exchange
Semantic Interoperability
Semantic interoperability in healthcare goes one step further. It ensures that the systems not only retrieve data but also understand and interpret the meaning. It’s used in multi-cloud platforms that enable scalable, centralized data exchange.
Trend #3: Ambient AI In Clinical Workflows
How would you feel if you were sharing your health concerns and your doctor was busy typing notes instead of listening?
That’s valuable time lost and expertise misused. But with ambient clinical intelligence (ACI), this hassle has gone away.
This AI-powered voice recognition technology uses natural language processing (NLP) and speech-to-text algorithms to capture the entire conversation between the doctor and the patient. It then automatically organizes and structures the information. By the time data enters your EHR system, it’s clean, accurate, and ready to use.
Benefits of Ambient AI in EHRs
- Supports advanced analytics
- Reduces administrative burdens for clinicians
- Reduced manual work and fewer errors
- Encourages human-in-the-loop AI for better decisions
Trend #4: Prior Authorization & Payer-Provider Automation
Patients often need prior authorization from insurance companies for tests, procedures, or medications. Before the modern EHR system architecture, hospitals had to wait for days or even weeks just to get an MRI approved.
Now, with modern EHR systems, hospitals no longer have to wait. The system connects directly to the payer’s FHIR APIs, sending requests, receiving responses, and updating patient records automatically.
The process works like this:
- Requests are sent instantly to insurance networks
- Approvals or rejections are updated in real time
- Transparent audit trail for compliance and trust
- No more faxing, just automated scripts
EHR prior authorization automation keeps patient care moving and ensures data stays secure in efficient workflows.
Trend #5: Cloud-Native & Zero-Trust Architecture
Many healthcare organizations still rely on outdated, monolithic EHR methods. But these legacy frameworks aren’t built for open, secure data exchange.
That’s why moving to the cloud has shifted from optional to essential. With microservices architecture in EHR development, hospitals get systems that scale easily, recover faster, and ship updates without breaking workflows.
But what happens if someone tries to access data they shouldn’t?
To prevent that, modern EHRs use zero-trust architecture. It follows a simple rule: never trust, always verify. Every user, device, or app has to continuously prove it’s allowed to access sensitive patient information, making EHR development far more reliable.
Features include:
- Continuous identity verification
- Segmented networks that limit breach impact
- Strict access policies that protect every data touchpoint
9 Out Of 10 Hospitals Have Adopted EHR Solutions. Have You?
What Are The Best Practices For EHR Software Development In 2026
Knowing what’s trending in healthcare is just one piece of the puzzle. The 2025 Workgroup for Electronic Data Interchange (WEDI) survey found that 52% of hospitals and clinics still haven’t started working on API requirements.
Why?
Because they’re struggling to align all the moving parts of interoperability, such as TEFCA, HIEs, and the shift towards FHIR EHR development.
Once you understand the core best practices behind modern EHR software development, it becomes much easier to build EHR system components that are scalable and stay compliant.
Some of the best practices are:

Design for FHIR & Version Resilience
- Use SMART on FHIR development with OAuth2 for EHR authentication and OpenID Connect in healthcare apps for secure app-level access.
- Map internal domain models to FHIR resources via a thin translation layer to stay future-proof across R4, R5, and beyond.
- Treat FHIR as API contracts, not storage schemas, to simplify upgrades and integrations.
Build Interoperability as a Product
- Adopt an API-first approach. Use versioned, discoverable APIs for every EHR feature.
- Ensure TEFCA-ready design with consent management, provenance, and standardized exchanges.
- Use automated test harnesses to emulate HIEs, payer APIs, and patient-facing apps to catch integration issues early.
Embed AI Safety & Responsibility
- Treat AI/LLM features as regulated subsystems with model governance in clinical AI.
- Implement privacy-first ML pipelines using embedding hygiene for clinical AI and differential privacy in EHR.
- Keep a human-in-the-loop AI for all clinical recommendations, showing confidence scores and source citations.
Prior Authorization & Payer Integration
- Automate prior authorization using payer API integration with FHIR-based APIs.
- Build dynamic interfaces reflecting real-time payer requirements.
- Track impact such as faster approvals, fewer touchpoints, and a compliant EHR audit trail.
Security, Compliance & Cloud-Native Readiness
- Use microservices architecture and EHR cloud deployment for scalable, event-driven workflows with FHIR subscriptions.
- Apply zero-trust principles like per-request auth checks, micro-segmentation, and immutable audit logs.
- Utilize service meshes and sidecars for strict access policies to ensure secure EHR development.
How to Develop FHIR-Based EHR Software in 2026: Practical Tips for Engineers
Even with best practices in hand, developers can face real-world challenges when building EHR systems. The tips below focus on the concrete steps engineers need to get things done efficiently and correctly:
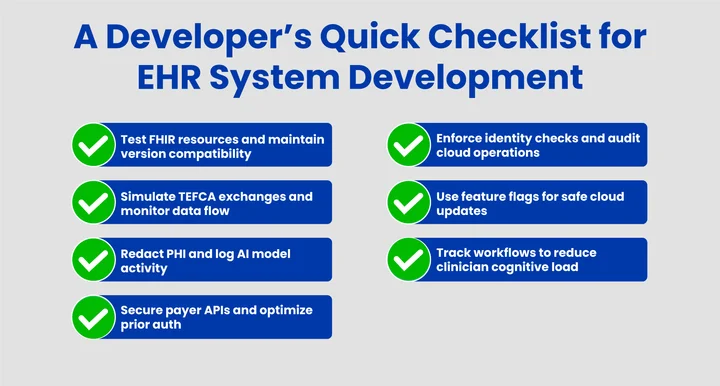
1. FHIR Implementation & Testing
Validate all FHIR resources with continuous integration tests, covering R4, R5, and custom profiles. Maintain automated migration paths to keep FHIR R4 and R5 compatibility in your EHR system.
2. Interoperability & TEFCA
Use mock HIEs or test harnesses to simulate TEFCA-ready exchanges and track consent, provenance, and document retrieval. Log metrics to monitor the quality of all TEFCA-aligned exchange flows in EHR interactions.
3. AI/LLM Pipelines
Reduce the vector indexing for embeddings or model training. Track model versions, input origins, and clinician overrides to ensure ML pipelines remain compliant and auditable.
4. Prior Auth Automation
Build secure endpoints for payer APIs including validation and fallback logic. Measure latency and retry rates with external payers to optimize prior authorization in EHR via payer APIs.
6. Security & Cloud Operations
Enforce per-service identity and token scopes, and implement append-only audit logs for traceable provenance. Deploy updates behind canaries or feature flags to maintain EHR service-mesh security and stability.
7. UX & Workflow Engineering
Measure clicks, task completion, and inbox load to reduce clinician cognitive burden. Use async background syncs and surface only relevant data at decision points to improve clinical workflow efficiency in EHR UX.
Conclusion: Building The EHR Of Tomorrow
The healthcare sector has never been more in the trenches. Patients are swarming, and doctors and clinicians are buried in admin work. Amid all this, the focus should remain on what matters most, which is treating patients with care. It becomes nearly impossible when you’re stuck with legacy systems or don’t have a proper EHR platform at all.
We’ve covered how electronic health records are evolving in 2026, how to implement these systems efficiently, and the key points your developers need to keep in mind. Now it’s your turn to turn this theory into practice.
Not sure where to start?
As a trusted healthcare software development company, Clustox has helped startups and enterprises build modern EHRs with experienced engineers and a carefully chosen technology stack. Let’s build an EHR system that’s scalable, secure, and clinician-friendly.
Frequently Asked Questions (FAQs)
2. What Are Common Pitfalls When Integrating AI Into EHR Workflows?
AI can overwhelm clinicians if not implemented carefully. Avoid skipping PHI redaction, model tracking, and human-in-the-loop checks. Keeping clear logs and transparent outputs ensures safe, regulatory-compliant AI adoption that actually helps, not hinders, care.
3. How To Ensure Ongoing Compliance And Security After EHR Deployment?
Security and compliance aren’t one-time tasks. Regularly audit logs, validate FHIR subscriptions, and monitor service-mesh policies. Continuous updates, zero-trust checks, and cloud-native deployment practices make sure your EHR stays secure as regulations and workflows evolve.
Tired of EHRs Slowing You Down?
Cut admin workload by up to 50% and focus on patient care.





Share your thoughts about this blog!