Have you noticed how much of our lives has gone digital lately?
I mean, we can order groceries, binge-watch shows, and video chat with friends without leaving the couch.
Healthcare is following the same trend. In fact, the digital health market is projected to soar to over USD 2.6 trillion by 2035, reflecting how quickly virtual care is becoming part of everyday life.
Imagine having a headache, and instead of heading to the doctor’s office, you simply grab your phone and get checked from your living room: no traffic, no waiting rooms, no magazines that smell a little… weird.
Sounds pretty convenient, right?
With telehealth and telemedicine, you can now access medical care and wellness support right from home, with no trips to the clinic and no waiting in line.
But here’s the thing: these terms are often used interchangeably, even though they actually cover different aspects of virtual care. Knowing the difference helps you make smarter choices about your health.
In this blog, we’ll break down the differences, peek at the tech behind them, and touch on the rules you need to know.
Table of Contents
Let’s get going!
What Is Telehealth, and How Is It Changing Patient Care?
If telehealth were a movie, it would be the blockbuster that covers everything: action, comedy, and drama all in one.
At its core, telehealth is “healthcare from a distance.” That means any service that helps you stay healthy, educated, or monitored without being in the same room as a healthcare professional.
The global telehealth market is expected to grow rapidly, reaching USD 180.86 billion by 2030, reflecting the increasing adoption of remote health services worldwide.
From checking in with a nutritionist to tracking your blood pressure from the comfort of your home, telehealth is all about making health easier to manage without hopping into a car or sitting in a crowded waiting room.
Applications of Telehealth
Telehealth shows up in more ways than you might think, from remote check-ins to full-on chronic care management.
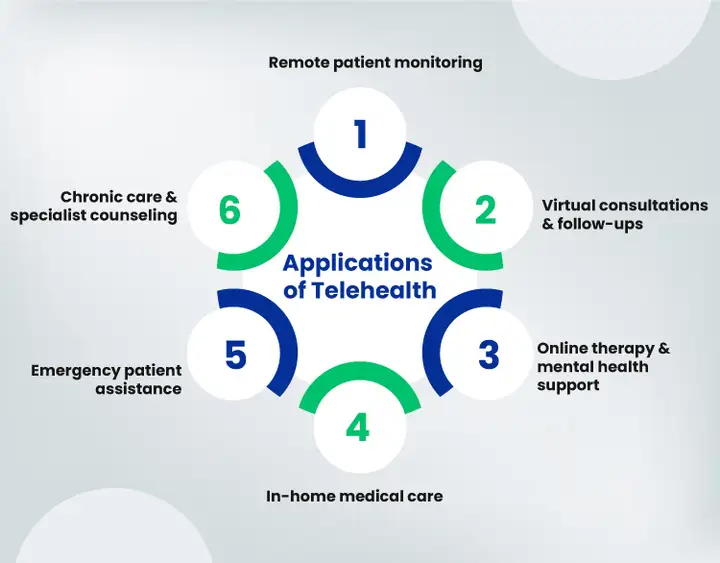
The following are just a few ways it’s changing the game:
- Remote patient monitoring.
- Teleconsultation and follow-up sessions.
- Remote psychotherapy and behavioral therapy.
- Remote home medical care and support.
- Patient care in emergencies.
- Specialized counseling systems for chronic conditions.
These applications show how telehealth keeps patients connected and supported, even when they’re miles away from a healthcare facility.
Telehealth gives you a taste of all the ways healthcare can reach you remotely, but when it comes to direct treatment and diagnoses, telemedicine takes the spotlight.
What Is Telemedicine, and How Does It Work in Healthcare?
If telehealth is the blockbuster movie with every storyline included, telemedicine is the thriller sequence: focused, high-stakes, and all about the action.
Telemedicine zeroes in on clinical care, meaning it’s all about diagnosing, treating, and managing patients remotely. Unlike telehealth, which covers wellness and education,
telemedicine is specifically for actual medical treatment.
According to McKinsey, 60% of patients find telemedicine more convenient than in-person visits, highlighting how remote medical services simplify healthcare access.
Think of it as seeing your doctor in real time, except you don’t leave your house. Telemedicine lets you get a diagnosis, review lab results, adjust medications, or follow up after a procedure, all through secure, compliant digital platforms.
Applications of Telemedicine
Telemedicine enables doctors and specialists to deliver medical services remotely through advanced tools and platforms.
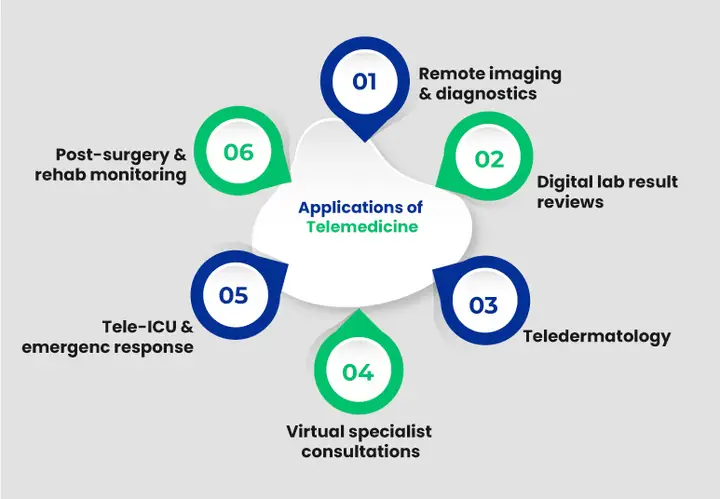
Common applications include:
- Remote imaging and diagnostics.
- Telepathology for lab result evaluations.
- Remote skin treatment (Teledermatology).
- Virtual consultations with specialists.
- Tele-ICU and emergency interventions.
- Post-surgery monitoring and rehabilitation care.
These applications highlight how telemedicine changes direct clinical care, offering patients timely access to expertise while ensuring safety and convenience.
What Are the Differences Between Telehealth and Telemedicine?
Now that we’ve seen telehealth and telemedicine individually, you might be wondering:
How are they really different?
Telehealth can be viewed as the full buffet, offering a variety of services to keep you healthy, while telemedicine is the main course, focused on providing the essential treatment you need when you’re actually sick. Both belong to the same virtual care universe, but each serves a distinct purpose.
To make it super simple, here’s a quick snapshot of their differences:
| Feature | Telehealth | Telemedicine |
|---|---|---|
| Scope | Broad: wellness, education, and monitoring | Narrow: diagnosis, treatment, clinical care |
| Purpose | Keeps you informed and supported in your health journey | Provides direct medical care and interventions |
| Services | Patient education, lifestyle coaching, remote monitoring, and teletherapy | Virtual doctor visits, ePrescriptions, tele-ICU, specialist consults |
| Healthcare Professionals Involved | Doctors, nurses, therapists, wellness coaches | Primarily, doctors and clinical specialists |
| Technology Focus | Apps, wearables, and video calls for monitoring & coaching | Secure platforms for clinical care, diagnostic tools, and patient record management systems |
| Regulatory Complexity | Moderate: fewer clinical regulations | High: must meet strict compliance, licensing, and data protection requirements |
In short, telehealth and telemedicine complement each other; one keeps you healthy every day, while the other steps in when medical care is needed. Together, they make virtual healthcare practical and reliable.
So from everyday wellness check-ins to getting a quick medical consult, you’ll know exactly which type of care fits the bill.
Up next, we’ll look at the software that keeps both running smoothly.
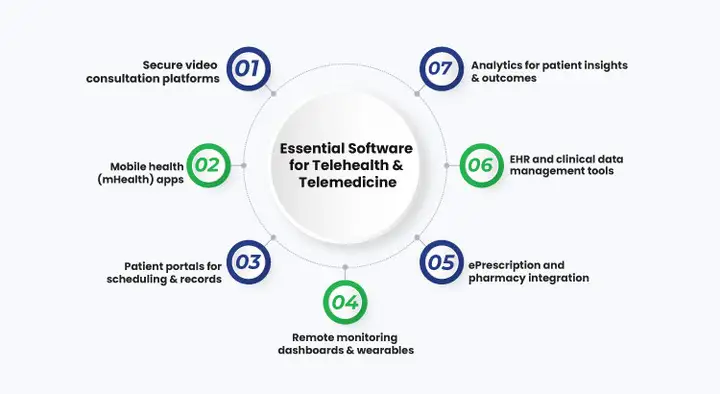
What Software Keeps Virtual Care Running Smoothly?
Alright, so how does all this actually work behind the scenes?
Just like you need the right utensils to cook a great meal, digital healthcare needs the right software to keep everything running smoothly.
These tools keep doctors and patients connected, data protected, and appointments running like clockwork. Without them, telehealth and telemedicine would just be fancy buzzwords instead of real, life-changing services.
Now we will discuss the technology that keeps it all running.
Telehealth Software: Supporting Wellness and Patient Engagement
Telehealth tools are all about wellness, engagement, and everyday care: the digital sidekicks that help you stay healthy between doctor visits. Think of them as your support system for everything before you actually need medical treatment.
Let’s take a look at the main types of software that keep telehealth running smoothly.
- Video Consultation Platforms
For chatting with your nutritionist, therapist, or coach without leaving the couch. These are your virtual meeting rooms for staying on track and motivated.
- Mobile Health Apps (mHealth Apps)
Your pocket-sized health assistant. From step counters to symptom trackers, these apps help you keep tabs on your well-being, remind you to take meds, and even cheer you on toward your fitness goals.
The right mobile app development team can help healthcare providers create secure, easy-to-use mHealth solutions that improve patient engagement and long-term wellness.
- Patient Portals
The one-stop shop for everything related to your health. View your records, book appointments, ask questions, or read up on medical info, all in one secure place.
- Remote Monitoring for Wellness
Wearables that track your sleep, heart rate, or daily activity. These tools help you and your care team spot small issues before they become big ones.
In short, telehealth software keeps you in the loop, helping you take charge of your health from anywhere.
Telemedicine Software: Clinical and Treatment-Focused Tools
Now here’s where things get a little more clinical: telemedicine software is what doctors use when it’s time for real treatment and diagnosis.
It’s like stepping into a digital clinic: everything your doctor needs to examine, treat, and monitor you safely is right there on screen.
This is the software doing the heavy lifting behind every virtual doctor visit.
- Secure Video Consultation Platforms
They’re HIPAA-compliant, encrypted, and designed specifically for medical visits, because privacy and accuracy matter when health decisions are on the line.
- ePrescription Systems
No more paper slips or pharmacy runs. Your doctor can send prescriptions straight to your pharmacy with just a few clicks. Convenient, fast, and error-free.
- Remote Monitoring Dashboards
For patients who need ongoing care, these dashboards stream real-time data, like blood pressure, glucose, or recovery stats, directly to their doctors. It’s like having your medical team watching out for you around the clock.
- EHR Integrations and Clinical Tools
From lab results to medical histories, all your data lives in one secure place. This helps doctors make smarter, faster decisions without digging through piles of paperwork.
If telehealth is the everyday helper, telemedicine software is the precision toolkit that powers real-time medical care.
The takeaway?
Both rely on smart tech, but telemedicine tools go deeper, adding clinical-grade features that help doctors diagnose, treat, and monitor safely, no matter the distance. With safe and trusted software solutions, patients and healthcare providers can enjoy secure, effective, and continuously accessible virtual care.
Still dealing with clunky apps that frustrate patients and staff alike?
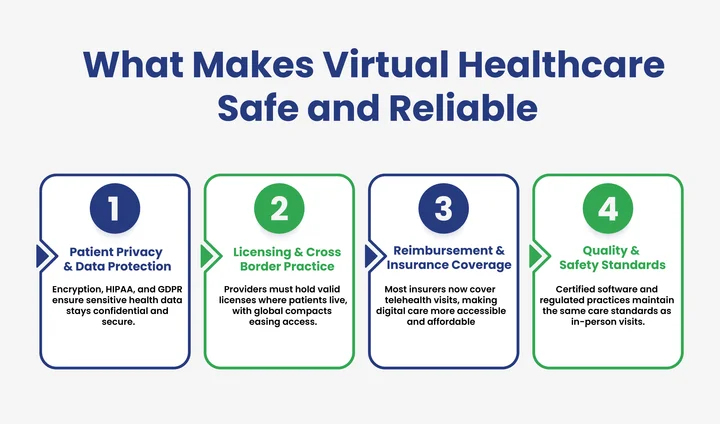
How Do We Keep Digital Healthcare Safe and Compliant?
When healthcare goes online, trust becomes everything. You’re sharing personal details, doctors are making decisions remotely, and sensitive data is flying through digital channels. That’s why both telehealth and telemedicine come with strict guardrails to keep everything private, legal, and secure.
So, how do these guardrails actually protect patients and providers?
Stick around to find out.
- Patient Privacy and Data Protection
Your health data is personal, and it should stay that way. Every message, video call, and file transfer must meet tough standards like HIPAA in the U.S. and GDPR in Europe.
It’s like a digital vault: only authorized people can unlock it, and everything inside is encrypted from end to end.
For telemedicine especially, secure storage and verified logins aren’t optional; they’re the backbone of patient trust.
- Licensing and Cross-State Practice
Here’s where things can get tricky. A doctor can’t just treat anyone, anywhere; they have to be licensed in the state or region where the patient lives.
Telehealth programs that focus on education or coaching have a little more wiggle room, but telemedicine, being clinical, follows much stricter rules.
For Example
In the U.S., the Interstate Medical Licensure Compact (IMLC) helps doctors get licensed in multiple states faster. That means a doctor in Maryland can treat patients in Pennsylvania or Virginia without waiting months for approval.
Similar initiatives are popping up around the world, making it easier for cross-border digital care to become the norm.
- Reimbursement and Insurance Coverage
Getting paid for virtual care used to be complicated, but that’s changing fast.
Most major insurers, and even government programs like Medicare and Medicaid, now cover telehealth and telemedicine visits, especially after seeing their success during the pandemic.
Still, coverage can vary by location and service type, so providers need to stay up-to-date with local regulations.
- Quality and Safety Standards
Just because care happens online doesn’t mean the standards drop. Doctors and clinics still have to document, follow up, and maintain the same quality as in-person visits.
Certified software and secure systems are necessary to ensure that patients get the same reliable care, just delivered through a screen instead of a stethoscope in the room.
Digital healthcare only works if people trust it.
The right tech, backed by strong privacy laws and evolving regulations, ensures that telehealth and telemedicine stay convenient, credible, and dependable.
Final Thoughts: Bridging the Gap Between Care and Convenience
Telehealth and telemedicine are two sides of the same story. One focuses on treating patients through virtual visits, while the other expands that idea, connecting care teams, patients, and data in one digital space.
Together, they’ve turned distance into connection and convenience into trust, proving that quality care doesn’t always need a clinic. What began as a way to reach rural patients is now shaping how everyday healthcare works.
Of course, with all that progress comes new responsibility: protecting patient data, meeting compliance standards, and ensuring that every click in a care app is as safe as a visit in person.
The good news?
The healthcare world is adapting quickly, with smarter systems, stronger privacy protections, and software built to meet the same standards you’d expect in a clinic.
Building a platform that works well for both patients and doctors requires reliable healthcare development services that ensure digital health solutions are secure and easy to use.
At the end of the day, it’s about how digital health makes care compliant and accessible to everyone who needs it.
Frequently Asked Questions (FAQs)
2. How Do Telemedicine Apps Integrate With Hospital Systems?
Telemedicine apps integrate with hospital systems primarily through electronic health record (EHR) platforms and other healthcare IT infrastructure. This integration ensures clinicians have access to patient data, lab results, and medical histories.
3. What Is the Typical Tech Stack for Telemedicine Software?
The technology stack for telemedicine software usually includes cloud hosting for secure data storage, video streaming frameworks for real-time consultations, and encryption protocols for data protection. It also relies on databases to manage patient records, APIs for EHR integration, and mobile/web front-end frameworks for patient and clinician access.
4. How Do Wearable Devices Support Telehealth Services?
Wearable devices collect health data such as heart rate, sleep patterns, blood pressure, and physical activity. This information is transmitted to healthcare providers through telehealth platforms, enabling remote monitoring and early detection of potential issues. Wearables help patients stay engaged with their wellness goals.
5. How Does Telehealth Software Support Mental Health Services?
Telehealth software enables virtual therapy sessions, counseling, and behavioral monitoring, making mental health support more accessible. Patients can connect with licensed therapists from home, track mood and progress through digital tools, and receive reminders for self-care activities.
Tired of compliance setbacks slowing your digital health growth?




Share your thoughts about this blog!