Did you know healthcare organizations generate more patient data today than ever before, but managing it efficiently remains a significant challenge?
In terms of patient safety, operational effectiveness, and care coordination, selecting the appropriate system can make all the difference.
So, what’s the difference between EMR, EHR, and PHR, and why does it matter?
EMRs keep records within a single clinic, EHRs let providers share data securely across networks, and PHRs empower patients to take control of their own health information.
With over 96% of U.S. hospitals using certified EHRs, it’s clear that integrated, secure, and accessible records are essential. Understanding each system helps healthcare leaders make more intelligent decisions that improve workflows, data sharing, and patient engagement.
In this blog, we will explore how healthcare organizations can make informed choices between EHR, EMR, and PHR systems.
Now, let’s begin by understanding what an Electronic Medical Record (EMR) is.
What Is an Electronic Medical Record (EMR), and How Does It Work in Healthcare?
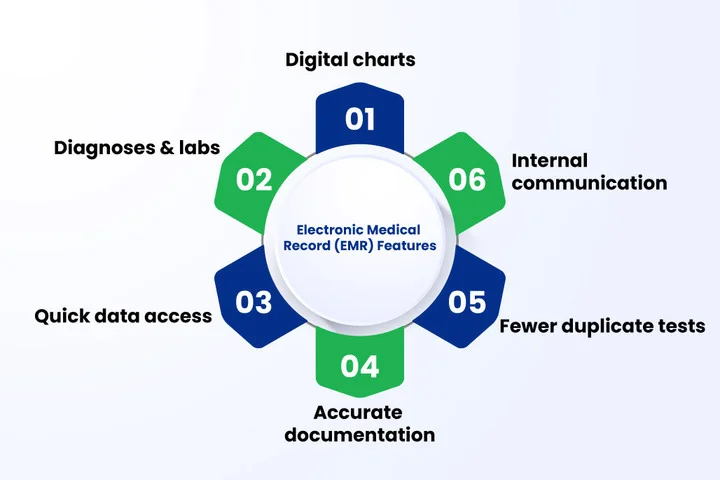
Table of Contents
To begin with, an Electronic Medical Record (EMR) is a digital version of a patient’s paper chart that stores information such as diagnoses, allergies, and lab results. It allows healthcare professionals to access data quickly, improving accuracy and reducing paperwork.
Furthermore, many hospitals rely on electronic medical record systems to simplify administrative tasks and improve treatment coordination. Using EMRs has been reported to result in fewer medical errors and faster access to critical patient data, both key indicators of improved care quality.
Benefits of EMRs for Healthcare Providers
EMRs offer several advantages that support everyday clinical operations:
- Better documentation accuracy through digital record-keeping.
- Quick access to patient data for timely decisions.
- Reduced duplication of tests and procedures.
- Improved internal communication between clinical departments.
Additionally, EMRs support health record integration within the same organization, allowing care teams to coordinate more efficiently.
Limitations of EMRs for Healthcare Providers
However, despite these benefits, EMRs also present a few limitations:
- Limited data sharing beyond a single healthcare facility.
- High implementation and training costs for smaller clinics.
- Challenges in achieving EHR interoperability.
- There are integration issues with newer digital health tools.
As a result, many organizations struggle to maintain data continuity when patients receive care from multiple providers.
Why Does It Still Matter Today?
Despite these challenges, EMRs continue to play an essential role in healthcare documentation. They remain the foundation of many electronic health record systems, helping providers digitize operations and ensure regulatory compliance.
Furthermore, for smaller practices, EMRs often serve as the first step toward complete digital transformation.
Struggling with scattered patient records and avoidable errors? Use a digital EMR system to centralize records and simplify patient data management.
What are Electronic Health Records (EHRs), and How Do They Improve Care Coordination and Data Sharing?
Moving forward, Electronic Health Records (EHRs) are comprehensive digital systems that store a patient’s medical data across multiple healthcare settings. Unlike EMRs, which are limited to a single organization, EHR systems enable doctors, specialists, and laboratories to securely and in real time share information.
This accessibility improves care coordination and ensures consistent treatment decisions, regardless of where a patient receives care. Implementing EHR solutions requires reliable cloud engineering services to provide secure and seamless data sharing across providers.
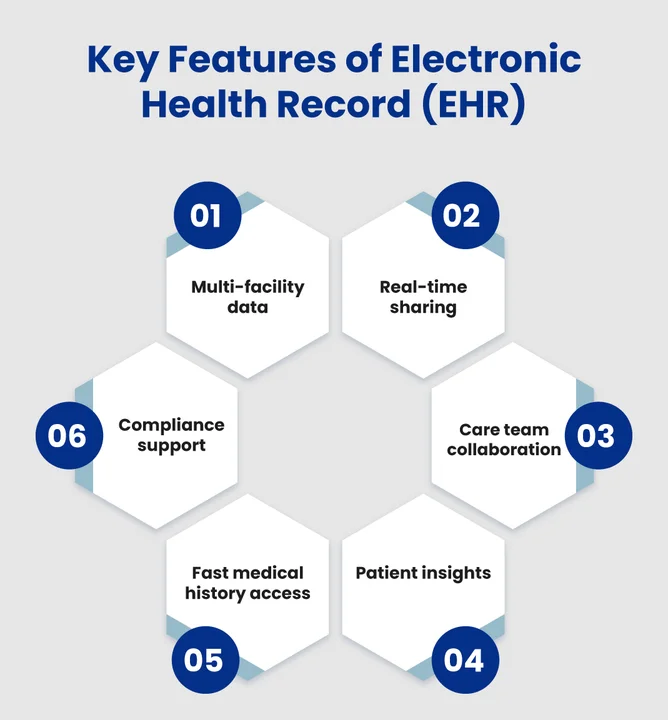
Benefits of EHRs for Healthcare Providers
Furthermore, EHRs offer several operational and clinical benefits, including:
- Improved collaboration among care teams through healthcare data sharing.
- Comprehensive patient insights for accurate diagnosis and treatment.
- Reduced paperwork and faster access to medical history.
- Simplified compliance with data protection standards like HIPAA.
Limitations of EHRs for Healthcare Providers
However, despite their broad adoption, EHRs also come with some limitations:
- High implementation costs and ongoing maintenance.
- Staff training challenges during system transitions.
- Data security concerns related to cloud access.
- Interoperability gaps between different vendors.
Why It Still Matters Today
Even with these challenges, EHRs remain essential for healthcare modernization. They improve health record integration, enable patient data portability, and foster a culture of connected, data-driven decision-making across healthcare networks.
Personal Health Records (PHRs): What are they, and Why Do Patients Need Them Now?

Personal Health Records (PHRs) are patient-managed digital platforms that store an individual’s complete health information in one accessible space, unlike Electronic Health Records (EHRs), which healthcare providers maintain.
PHRs are controlled directly by patients, giving them ownership over their medical data. These records can include details such as medical history, prescriptions, lab results, allergies, and vaccination records, all accessible anytime, anywhere.
Benefits of PHRs for Patients
PHRs empower patients to take an active role in their healthcare by enabling them to:
- Access and update their health information independently.
- Share data easily with multiple healthcare providers or family caregivers.
- Track chronic conditions, medications, and lifestyle metrics to stay informed and manage your health effectively.
- Receive personalized insights and reminders for checkups or medications.
Limitations
Despite their advantages, PHRs also face certain limitations:
- Limited integration with healthcare providers’ EHR systems.
- There are privacy and security risks if data isn’t properly encrypted.
- Varying levels of digital literacy among patients.
- Lack of standardized data formats across platforms.
Why They Matter Now
In today’s digital-first healthcare environment, PHRs are becoming increasingly vital. They promote transparency, improve patient engagement, and ensure continuity of care, especially in telehealth and remote monitoring scenarios. As healthcare shifts toward patient-centered models, PHRs are essential for fostering informed, proactive, and data-aware patients.
EHR vs. EMR vs. PHR: The Differences and How to Choose the Right System
As healthcare data grows more complex, understanding the differences between EMR, EHR, and PHR systems is key to making the right technology decisions. While all three aim to improve documentation and care coordination, they vary in scope, control, and interoperability.
The table below highlights the differences in management, accessibility, and purpose of these systems within the healthcare ecosystem.
| Feature | EMR (Electronic Medical Record) | EHR (Electronic Health Record) | PHR (Personal Health Record) |
|---|---|---|---|
| Managed by | Single healthcare provider or clinic | Multiple providers and healthcare organizations | Patients |
| Data Scope | Clinical data within one organization | Comprehensive data across various care settings | Personal health and wellness data managed by the individual |
| Access Level | Limited to internal clinical staff | Accessible to authorized providers and sometimes patients | Fully controlled by the patient |
| Primary Purpose | Internal recordkeeping and documentation | Care coordination and data sharing | Patient engagement and self-management |
| Integration Capability | Restricted to in-house systems | High interoperability across networks | Depends on platform compatibility |
In essence, EMRs focus on managing patient information within a single healthcare facility, while EHRs extend that data across multiple providers to enable seamless coordination and continuity of care. PHRs, meanwhile, give patients complete control over their own health data, fostering greater engagement and transparency.
Together, these systems represent different layers of healthcare digitization, each serving a distinct purpose in improving efficiency, collaboration, and patient participation.
How to Choose the Right Health Record System for Your Organization?
Choosing between EMR, EHR, and PHR depends on your organization’s size, workflow, and care goals. Each serves a different purpose: EMRs simplify internal documentation, EHRs improve data sharing, and PHRs increase patient involvement.
Important Factors to Consider:
- Scope: EMRs suit smaller clinics, while EHRs fit larger networks with multiple providers.
- Interoperability: For effortless data exchange, EHRs offer stronger integration.
- Patient Engagement: If your focus is on empowering patients, PHRs add value.
- Security & Compliance: Ensure the system meets HIPAA and data protection standards.
- Budget: Evaluate setup, training, and maintenance costs before implementation.
In many cases, a blended approach, using EMRs for internal workflows, EHRs for collaboration, and PHRs for patient access, delivers the best balance between efficiency and engagement.
Frequently Asked Questions (FAQs)
2. Can EMR and EHR Systems Work Together in One Healthcare Setup?
Yes, but integration can be complex. Many organizations use EMRs for internal clinical operations and connect them with EHRs for broader care coordination. Achieving this connection often depends on vendor compatibility and cloud infrastructure that supports secure data exchange.
3. How do Personal Health Records (PHRs) Improve Patient Engagement?
PHRs provide patients with direct access to their health information, enabling them to track medications, monitor their conditions, and share updates with multiple healthcare providers. This transparency strengthens trust and encourages patients to take a more active role in their treatment and preventive care.
4. What Factors Should Healthcare Providers Prioritize When Implementing a New Record System?
Key priorities include:
- Scalability for future growth.
- Data security and privacy compliance.
- Interoperability across systems.
- Staff training for smooth adoption.
- Alignment with long-term digital goals.
Summary: Building a Smarter, Connected Health Record Strategy
Healthcare organizations today face a growing challenge: managing vast amounts of patient data while ensuring accuracy, privacy, and accessibility. Selecting the right health record system plays a crucial role in addressing these issues and enabling more coordinated, data-driven care.
As the shift toward cloud infrastructure accelerates, scalability and interoperability are becoming key considerations. Many healthcare providers are now adopting the right cloud platforms for healthcare, such as AWS, Azure, and Google Cloud, to support secure and compliant data management.
By combining the right record system with a robust cloud foundation, healthcare organizations can create a more innovative, more connected ecosystem that enhances both operational efficiency and patient outcomes.
Struggling with scattered patient records? Centralize records, increase efficiency by 45%, and cut errors by 65% with the right patient management system.






Share your thoughts about this blog!