With the rapid digitization of patient records, technical safeguards under HIPAA have become more than just regulatory jargon because they are mission-critical shields for protecting sensitive data. In the HIPAA Journal’s Healthcare Data Breach Report 2024, more than 133 million healthcare records were exposed in 2023, marking one of the worst years on record for data breaches.
With such staggering breaches highlighting the risks, it’s clear that healthcare organizations need more than basic security measures.
But what exactly do HIPAA’s technical safeguards require to truly protect sensitive patient data?
It’s not enough to rely on basic security measures. In healthcare, organizations must implement access controls, audit trails, encryption, and authentication systems that meet HIPAA’s rigorous standards.
Yet, many providers continue to struggle with interpreting and applying these requirements effectively.
So, where does compliance end and true protection begin?
How can healthcare organizations bridge the gap between “checking the box” and building resilient security practices?
Let’s investigate this further in this blog so you can learn more!
Table of Contents
The HIPAA Security Rule: Core Foundations Explained
The HIPAA Security Rule establishes the framework that healthcare organizations must follow to protect electronic protected health information (ePHI). Its central purpose is to ensure the confidentiality, integrity, and availability of patient data, which are the three pillars that guide every safeguard requirement.
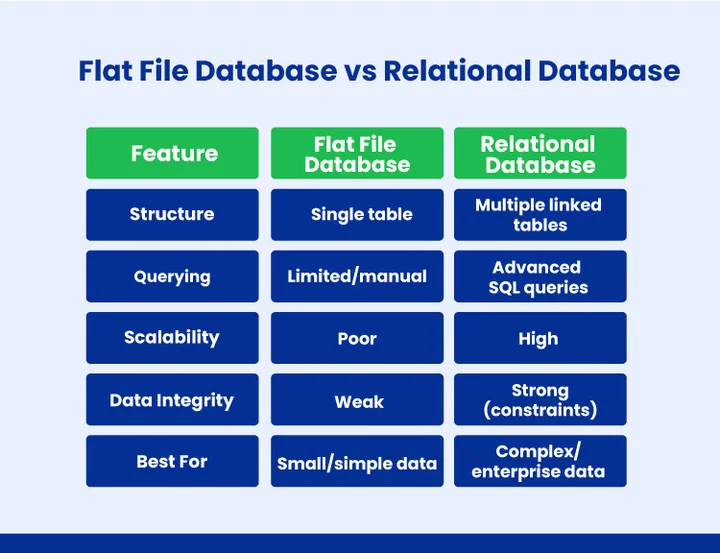
Unlike the HIPAA Privacy Rule, which governs who may access information, the Security Rule focuses on how that data is secured from unauthorized access, alteration, or loss. At its core, the rule rests on three foundational safeguard categories, each addressing a different layer of protection:
- Administrative Safeguards: Policies, procedures, and workforce training that ensure security practices are consistently followed.
- Physical Safeguards: Facility access controls, device protections, and physical measures to prevent unauthorized access to systems and equipment.
- Technical Safeguards: Technology-based controls such as access restrictions, audit trails, encryption, and authentication to protect ePHI in digital environments.
Together, these foundations create a multi-layered defense. Organizations that understand and implement all three safeguard types not only meet compliance requirements but also strengthen resilience against cyber threats and data breaches.
Among these, technical safeguards form the backbone of HIPAA compliance in digital environments. Let’s break down exactly what they require.
Struggling to implement HIPAA safeguards across your HealthTech systems?
What Exactly Do HIPAA Technical Safeguards Require?
The HIPAA Security Rule outlines specific technical safeguards that covered entities and business associates must implement to protect electronic protected health information (ePHI). These safeguards serve as the technological backbone of HIPAA compliance and aim to ensure data confidentiality, integrity, and availability.
Here are the core requirements every organization should address:
- Access Controls: Covered entities must establish technical policies and procedures that only allow authorized individuals to access ePHI. This includes unique user IDs, emergency access procedures, and automatic logoff features.
- Audit Controls: Systems must be equipped to record and examine activity, enabling organizations to detect unauthorized access or unusual patterns of use.
- Integrity Controls: Technical measures are required to ensure ePHI is not improperly altered or destroyed, whether intentionally or by accident.
- Authentication: Verification methods (such as passwords, PINs, or multi-factor authentication) must be in place to confirm that users or systems accessing data are legitimate.
- Transmission Security: Organizations must safeguard ePHI during electronic transmission by using encryption or other protective mechanisms to prevent interception.
Taken together, these safeguards form the foundation of HIPAA’s technical compliance framework. While some elements are marked as “required” and others as “addressable,” ignoring them exposes healthcare organizations to compliance violations, financial penalties, and reputational harm.
More importantly, they play a direct role in reducing risks from modern threats such as ransomware and phishing attacks.
How to Implement These Safeguards in Practice?
HIPAA does not prescribe specific tools but expects organizations to apply safeguards in a way that fits their size, resources, and risk level. Here’s how each safeguard can be put into practice:
- Access Controls: Use role-based access management and multi-factor authentication (MFA).
- Audit Controls: Deploy log monitoring and auditing solutions (e.g., Splunk, ELK Stack).
- Integrity Controls: Implement checksums, file integrity monitoring, and automated alerts for unauthorized changes.
- Authentication: Require strong passwords, biometric checks, or MFA for system logins.
- Transmission Security: Encrypt data in transit with TLS/SSL and secure VPNs.
Even small steps like MFA or automated log monitoring significantly strengthen compliance and reduce breach risks.
Required vs. Addressable Safeguards: What’s the Difference?
While all the technical safeguards listed above are important, HIPAA categorizes them into two types: required and addressable. Understanding this distinction is crucial for organizations to apply safeguards effectively, prioritize resources, and avoid compliance gaps.
1. Required Safeguards
These safeguards must be implemented exactly as stated in the HIPAA Security Rule. There is no flexibility or alternative option; failing to comply constitutes a direct violation. Examples include establishing access controls and ensuring proper authentication measures.
2. Addressable Safeguards
Addressable safeguards provide some flexibility. Organizations must assess whether implementing a safeguard as written is reasonable and appropriate, considering their size, resources, and risk environment.
If the exact safeguard isn’t feasible, an organization can adopt an equivalent alternative, but it must document the decision and the alternative measures.
Healthcare companies can enhance their security posture, mitigate risk exposure, and maintain regulatory compliance by comprehending and effectively implementing both necessary and addressable safeguards.
What are the Common Challenges in Meeting HIPAA Technical Safeguards?
Even with clear guidelines, many organizations struggle to meet HIPAA’s technical safeguards. Budget limitations often prevent smaller providers from upgrading outdated systems, leaving them exposed to risks. Misunderstanding “addressable” requirements is another challenge, as some assume these controls are optional rather than flexible.
In addition, a lack of regular staff training increases the chances of errors, while legacy EHR systems make it harder to integrate modern security measures effectively. The most frequent challenges include:
- Limited Budgets & Outdated Systems: Smaller providers often lack funds to upgrade aging IT infrastructure, making compliance harder.
- Misinterpreting “Addressable” Requirements: Many mistakenly assume “addressable” means optional, creating dangerous security gaps.
- Lack of Staff Training: Without proper awareness, employees may mishandle ePHI or fall for phishing attempts.
- Legacy EHR Integration: Older record systems can be difficult and costly to secure with modern safeguards.
Frequently Asked Questions (FAQs)
2. What is the Purpose of Technical Security Safeguards?
Technical security safeguards protect electronic protected health information (ePHI) by controlling access, ensuring data integrity, monitoring activity, and securing data during storage and transmission. Their purpose is to prevent unauthorized access, data breaches, and cyber threats while supporting HIPAA compliance.
3. How Do “Required” and “Addressable” Safeguards Differ?
HIPAA distinguishes between safeguards that must be strictly applied and those that allow some flexibility:
- Required: Must be implemented exactly as HIPAA states.
- Addressable: Flexible; implement if reasonable, or use an alternative and document it.
4. How Do Technical Safeguards Help Prevent Data Breaches?
Technical safeguards lower the risk of unauthorized access, ransomware attacks, and other cyber threats by limiting who can access ePHI, keeping an eye on system activity, confirming user identities, preserving data integrity, and securing transmissions. This ensures compliance and protects patient data.
Summary
In the end, HIPAA’s technical safeguards are about building security practices that truly protect patients from today’s cyber risks. With the rise of healthcare data breaches, it’s clear that simply knowing HIPAA rules isn’t enough. Organizations need practical ways to protect sensitive patient information.
How can healthcare providers ensure their ePHI stays secure while remaining accessible to the right people? Implementing technical safeguards like access controls, audit trails, authentication, and secure transmission are the essential first steps. These measures not only reduce the risk of cyber threats but also help maintain trust and operational efficiency.
But applying safeguards effectively can be challenging, especially in complex or legacy systems. One practical approach is to integrate reliable processes and monitoring into your infrastructure.
For instance, DevOps services provide structured, technology-driven solutions that support secure system management, making it easier to uphold HIPAA requirements daily. By combining the right safeguards with thoughtful system practices, healthcare organizations can move beyond compliance toward a truly resilient and secure digital environment.
Protect Your HealthTech Systems and Safeguard Patient Data!





Share your thoughts about this blog!