Why do so many promising AI pilots in healthcare lose momentum before ever reaching real patients?
It’s a question that frustrates both innovators and clinicians alike. After months of data gathering, testing, and fine-tuning, progress often stalls just as results start to look promising.
However, even when AI pilots perform well in controlled environments, scaling them across hospital systems presents an entirely new challenge. Data stays fragmented, regulations are complex, and many clinicians remain cautious about trusting AI-driven insights in real-world care.
At its core, this clearly shows that early success in a pilot phase doesn’t always guarantee lasting impact in real clinical settings.
In this blog, we will explore why many healthcare AI projects stall, what causes healthcare AI pilot failure, and how successful projects move beyond the pilot stage.
So, let’s get started.
What Are the Main Reasons AI Pilots Stall in Healthcare?
To begin with, it’s no secret that launching an AI pilot in healthcare is only the first step. Many organizations celebrate early successes, but scaling these projects into full deployment often proves much harder than anticipated.
This gap raises an important question: what exactly causes promising AI initiatives to stall before they can deliver real impact?
Table of Contents
Moreover, understanding these barriers is essential for any healthcare provider aiming to implement AI consulting solutions effectively. Challenges can arise from multiple angles, including technology, data, and even human factors.
For instance, even the most accurate AI implementation in healthcare can fail if clinicians don’t trust or adopt it in their daily workflows.
Facing roadblocks in scaling your AI pilot? Our experts help you integrate data, gain clinician trust, and deliver measurable results.
So now, let’s take a closer look at the specific reasons most AI pilots in healthcare struggle to move forward.
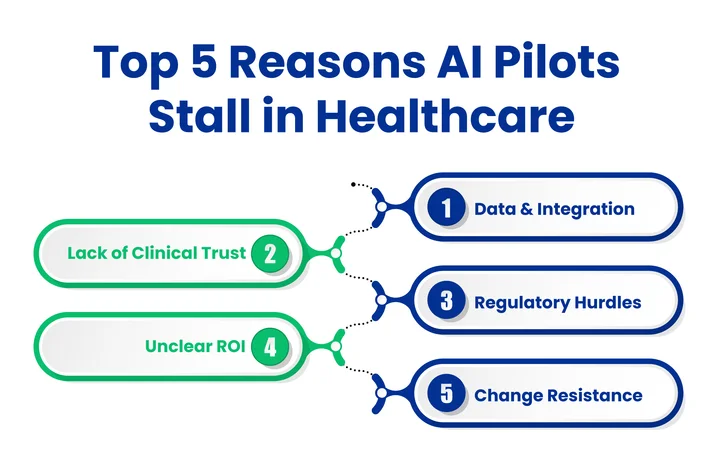
1. Tackling Data and Integration Challenges
Let’s face it: healthcare data is scattered across multiple systems and formats, creating real hurdles for AI pilots. This fragmentation makes it difficult to connect new tools to existing workflows effectively.
On top of that, incomplete or inconsistent information can reduce model accuracy, making clinicians hesitant to rely on AI in healthcare.
Moreover, a smooth AI workflow integration relies on accurate, well-structured data. Missing patient records or incompatible formats can prevent pilots from showing meaningful results.
Furthermore, integrating AI solutions with electronic health records and other hospital systems often takes longer than expected, thereby delaying the broader deployment of healthcare AI.
Notable Challenges include:
- Inconsistent data formats across departments and systems
- Healthcare data fragmentation AI limits pilot effectiveness
- Difficulty integrating AI pilots in healthcare with electronic health records
To overcome obstacles in the clinical adoption of AI in healthcare, it is necessary to cultivate clinician confidence.
Now that we understand how data and integration hurdles can stall scaling AI in healthcare organizations, the next factor to explore is clinician trust and adoption.
2. Lack of Clinical Adoption and Trust
Clinicians play a significant role in determining whether an AI pilot in healthcare succeeds. Even highly accurate AI implementation in healthcare can stall if staff don’t fully trust or understand its recommendations.
Moreover, AI tools that disrupt existing workflows or create additional tasks often face resistance. Limited exposure to AI and unclear communication can slow down adoption.
There are several obstacles:
- Limited understanding of AI decisions
- Concerns over reliability
- Disruption to daily clinical workflows
Overall, fostering clinician confidence is essential to ensure that healthcare AI deployment moves beyond the pilot phase.
3. Handling Regulatory and Compliance Hurdles
Healthcare organizations face strict rules when implementing AI. Even models that perform well in testing can take longer to implement due to compliance hurdles.
The primary standards and regulations are:
- HIPAA: Protecting patient health information and privacy
- FDA approvals: For AI/ML-based medical devices (SaMD)
- HITECH Act: Ensuring secure electronic health records
- GDPR: Handling international patient data and privacy
- 21 CFR Part 11: Requirements for electronic records and signatures
- ISO 13485: Quality management standard for medical devices
These compliance checks affect how quickly AI tools can be integrated into real clinical workflows. Hospitals must ensure data privacy, protect sensitive patient information, and meet reporting and validation requirements before scaling AI solutions.
Ultimately, understanding and proactively addressing these regulatory and compliance requirements is critical for any AI implementation in healthcare that aims to move beyond the pilot stage.
4. Unclear ROI (return on investment) and Organizational Misalignment
Even when an AI pilot in healthcare performs well technically, it can stall if the benefits aren’t clearly visible. Without measurable outcomes, decision-makers struggle to justify scaling, and promising projects risk being shelved.
Additionally, misalignment between leadership, IT, and clinical teams often creates confusion, as differing expectations and priorities can slow progress, leaving pilots stuck in limbo. Short-term pressures to reduce costs may overshadow long-term gains, preventing the organization from realizing the full potential of AI implementation in healthcare.
In the end, defining clear objectives and aligning all stakeholders is essential to ensure healthcare AI deployment moves beyond experimentation and delivers real impact for patients and providers.
5. Change Resistance Across Teams
Even when technology works flawlessly, organizational culture can stop an AI pilot in healthcare from progressing. Teams often work in silos, with IT, data scientists, and clinicians having different priorities. This disconnect can slow adoption and prevent pilots from reaching full healthcare AI deployment.
Moreover, staff may resist new workflows or fear that AI will replace existing roles. Without proper communication, training, and involvement from all stakeholders, even promising projects can stall.
To ensure AI adoption in healthcare advances from pilot testing to practical impact, it is imperative to promote collaboration, cultivate a culture of learning, and involve all teams in decision-making.
Now that we understand why most AI pilots in healthcare stall, it’s essential to see what allows some projects to scale successfully.
How Do Successful Healthcare AI Pilots Move Beyond the Pilot Phase?
It takes more than just encouraging outcomes to turn an AI pilot into a fully implemented healthcare solution. It demands structure, collaboration, and precise alignment with clinical and organizational goals. Successful deployments follow structured strategies addressing both technical and human factors.
Successful organizations typically focus on:
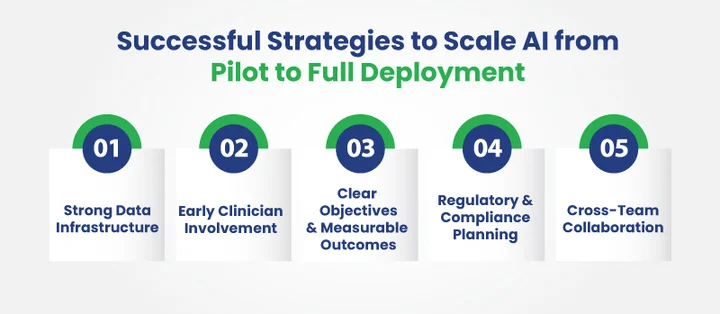
- Strong Data Infrastructure: It ensures patient information is clean, structured, and accessible across systems, supporting the integration of healthcare AI workflows. Hospitals with integrated data systems are twice as likely to scale AI pilots effectively, supporting smooth AI workflow integration.
- Early Clinician Involvement: Engaging medical staff from the start helps build trust and improve adoption. A survey report shows that 79% of healthcare professionals believe AI can enhance patient outcomes, yet only 38% feel current AI tools truly meet real-world needs.
- Clear Objectives and Measurable Outcomes: Defining goals and ROI metrics ensures leadership support and aligns the project with organizational priorities.
- Regulatory and Compliance Planning: Addressing HIPAA, FDA, and other requirements from the beginning reduces delays and mitigates risk, as highlighted by HIMSS insights.
- Cross-Team Collaboration: Encouraging communication among IT, clinical teams, and leadership ensures a shared understanding, increasing the likelihood that pilots will move into full-scale healthcare AI deployment.
In short, applying these strategies transforms pilots from isolated experiments into solutions that deliver real impact for both patients and providers.
Frequently Asked Questions (FAQs)
2. What are the Common Barriers to Scaling AI in Healthcare Systems?
The main barriers include:
- Inconsistent or incomplete patient data
- Limited clinician adoption or trust
- Complex regulatory and compliance requirements
- Misaligned organizational priorities
- Change resistance across departments
Addressing these factors early is essential for moving from pilot to full deployment.
3. How Can Healthcare Organizations Move From an AI Pilot to Full Deployment?
Successful deployment requires:
- Strong data infrastructure and integration with electronic health records
- Early engagement and training of clinicians
- Clear objectives, measurable ROI, and stakeholder alignment
- Proactive compliance planning
- Cross-team collaboration between IT, clinical, and leadership teams
4. How Can Healthcare Organizations Ensure Clinician Buy-In for AI Implementation?
Clinician buy-in is built by:
- Involving medical staff early in the AI design and testing process
- Communicating AI decision-making clearly and transparently
- Ensuring AI tools enhance, not disrupt, daily workflows
- Providing training and ongoing support
Trust and adoption increase when clinicians see measurable improvements in patient care.
5. How Do Governance and Compliance Impact Scaling AI in Healthcare?
Patient safety depends on regulatory requirements such as HIPAA, FDA approvals, and data privacy laws, but if these are not anticipated, they may delay AI adoption. Organizations that integrate compliance checks from the beginning reduce delays, mitigate risks, and ensure that AI solutions can be safely scaled across hospital systems.
Final Takeaway: Bridging the Gap from Pilot to Real Impact
Many AI pilots in healthcare show early promise but stall before full deployment due to fragmented data, limited clinician adoption, and unclear ROI. To turn pilots into long-term solutions, we must first understand these challenges.
Focusing on a solid data foundation, building clinician trust, and aligning organizational goals can all help increase success. Implementing AI and ML solutions thoughtfully enables healthcare teams to quickly integrate insights into daily workflows, enhancing decision-making and patient outcomes.
Additionally, a solid cloud infrastructure helps ensure reliable data management and compliance, enabling AI models to achieve the accuracy and consistency they need. By addressing these core areas, healthcare organizations can transform pilots into practical solutions that deliver measurable impact.
With the right approach, the gap between pilot projects and full-scale deployment can be bridged, enabling healthcare providers to leverage AI effectively for better patient care and operational efficiency.
Worried your AI pilot won’t scale due to compliance hurdles or unclear ROI?




Share your thoughts about this blog!